Memorial Day weekend ends up being a memorable weekend indeed.
Week 40 yoga: mummy and baby are happy co-residents. No sign of eminent departure. No eviction notice issued. We didn’t know it at the time, but we were t minus 7 days.
DAY 1:
Week 40 plus 5 days: Friday 5/27 at 1:30 am Premature Rupture of Membranes (PROM)… Wake up husband! Call the midwife! Call Nana! Text doula! A few contractions throughout the night. Clearly I’m new at this. I’ve heard women tell me their water broke in the night or that contractions started and they didn’t wake their husbands because they knew it would be a long while yet. Instead they did a few loads of laundry, and cleaned the house. That was definitely not me! I had joked I hoped to go into labor at work so I could be paid to do the work and also have the distraction. That was also definitely not me! I woke up everyone!
I was able to be fit in for an acupuncture appointment at my midwife’s clinic last minute for that morning at 10:30am, so we put the hustle on my quick breakfast of InstaPot steel cut oats and hurridly dressed in our french team VanLaanen outfits. We headed up to Wallingford on foot, and kept on walking all day. During the acupuncture session Dr. Ashley Landbloom ND LAc stimulated labor inducing points, and placed some super tiny needles (2mm long!) meant to be left in covered with a small round bandage for us to use to continue stimulating as needed after the visit. These were down near my ankles. She also placed one in each thumb web to help manage pain of contractions. Boy, did I use those ones a ton! We ended up turning in an eight mile walk of Greenlake and environs that day. Contractions were light, less than a minute about every 10 minutes. Given the PROM we were on a timeline and were given 24 hours to get labor rolling. Without the use of Ptosin (oxytocin) available to us, as midwifes’ scope of practice limits the use of Ptosin for emergency use in hemorrhage situations, not for labor induction, we had to get creative!
Friday afternoon 16 hours post PROM our rockstar midwife from Ground Floor Health in Wallingford, Carly Meiser, LM CPM, met us out at Mykonos Greek Grill the restaurant by Greenlake where we were eating lunch to bring us the labor plan including the requisite supplies. It was time to get serious. The 1am deadline is approaching quickly. We make it just under the wire. Right at midnight, my contractions started coming every 5 minutes lasting a minute or longer! Woo hoo! But woooooooo… Intense!!! We used the pressure points a lot! My mother and husband were amazing and continued to be even more so throughout the process.
DAY 2:
Saturday afternoon : Getting serious with the rebozo!
Saturday was all about keeping the contractions going and getting through them. At 5pm approximately 40 hours post PROM labor stagnated. We made some heroic last efforts with the rebozo and walking along the curb, but it wasn’t sufficient. We could technically wait until midnight, but decided it was unlikely things would progress enough over the course of the evening. Plus waiting until the last minute would just limit our options if we did transfer at that point. After calling the University of Washington Medical Center, the hospital one mile away that I had interned at, our original plan if hospital transfer was required, they were full and referred us to another UW Medicine entity, Northwest Hospital. I cried and tried not to think too much about how my friend jokingly calls it Northworst, but knew it was the right thing to do. I needed help. My body wasn’t ready for this on it’s own. We transfer to Northwest Hospital Childbirth Center. It was an excellent choice for many reasons. It was super quiet over the holiday weekend. One other room was occupied when we arrived. Ditto when we discharged. I was nonetheless a ball of nerves. I remember telling Dr. Solerno the attending physician who admitted me, “I really don’t want a Cesarean section.” I was petrified. And super concerned that adding on interventions would catapult me in that direction. She listened and heard me and said they had two goals at NWH: 1. Safe delivery for baby and mama, 2. Vaginal delivery. Then one of the nurses lightened the mood by saying, “We can promise you one thing: you won’t leave here pregnant!”
I got my IV port placed, and it was super uncomfortable on the distal left arm right over the lateral radius. I asked them to replace it, and I was really glad I did since it stayed in for several days. Right away they started bolusing one liter of Lactated Ringers for hydration. Within an hour the attending physician had me started on the Ptosin IV drip. Here their policy is to start low and go up slowly every half hour until the contractions are 2-3 minutes apart and significant and 1-1 1/2 minutes duration. The anesthesiologist came in to introduce herself and to say she was about to go into surgery so she wouldn’t be available for a bit. She wanted to offer/ask if I wanted an epidural placed before it might be more difficult to sit still, and that it would then be there if I needed it. I perseverated on this for several hours. I was doing okay and didn’t want to impede progress, but also was so scared of the intensity of the Ptosin generated contractions.
“I’m an anesthesiologist, you’re a pharmacist… Better living through chemistry,” she said. Of course I’m having really intense contractions by the time I ask for the epidural to be placed. We get through it with the help of the nitrous oxide.
DAY 3:
Ultimately: Birth-day!
They sleep me through the night getting me through active labor watching my cervix dilate up to the full 10 cm. at one point in the late morning the doctor measures me and says “I’m going to call that 9.8 cm and fully effaced. There’s a small right anterior lip. You could start pushing now, but it’s going to be more work, so why would you want to do that when we can just wait for the Ptosin to finish the job. We’ll start pushing at 1:30pm.”
So I gathered my crew, just in time to fire them all later. Turns out for me I liked a lot of support for contractions, but pushing was a pretty solitary affair. Just my husband and the rockstar OB, Dr. Ali Lewis. She called herself a wannabe midwife and had the medical student Autumn and one of the new nurses assisting. Both of them were sweating bullets while I leaned on them. Dr. Lewis had me pushing my feet into their chests, one on each side, like a modified happy baby. It was a bit awkward because due to my epidural I didn’t have enough strength in my left leg to walk or be on my hands and knees. I pushed for 3 1/2 hours. I pushed so hard, I remember asking Dr. Lewis if women ever stroke out or have their eyes pop out of their head when they are pushing. She reassured me that the most that happens is broken blood vessels in the eye.


My husband was amazing. He definitely got me through it. And the prize came at the end. But at that point I could barely see straight. Bless Amy the RN for getting him introduced to the breast right away. He was a swell sport and was happy to latch right away. A good eater right out of the gate!
DAY 4:
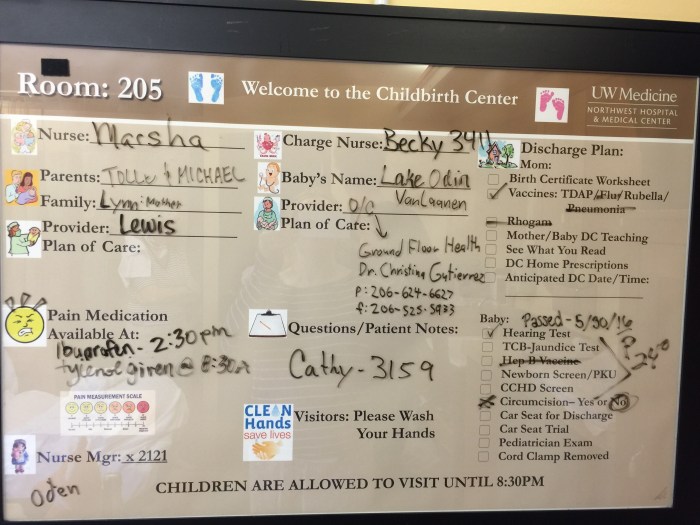
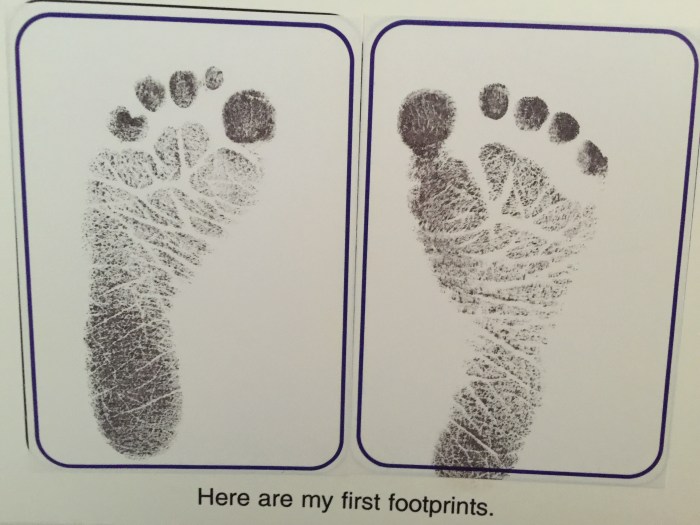
Waiting out 48 hour postpartum sepsis watch. We had a lot of tests done today. Angel assessed his hearing (he passed). He had his heel stuck for PKU and hypothyroidism. He had his forehead scanned for jaundice and bilirubin levels. He was assessed for cardiac defects. He had his footprints taken. People started remarking he had red hair. I couldn’t tell at this point. Things were still a bit of a blur. I felt like I’d been run over by a truck. Initiating movements were especially painful. I requested a lactation consultant come to help with feedings. I had a really hard time moving which made the micro-adjustments breastfeeding positioning requires really difficult. All my little muscles and ligaments in my back and hips had been strained to the max. He was a trooper, and even entertained his aunt coming to visit.
DAY 5:
The night was hard. Rock-bottom hard. My husband calls the night nurse because I’m crying uncontrollably. It’s so painful to move I can’t get to the bathroom. My son is next to me. I’m responsible for this tiny being. The night nurse Marsha looks to be in her sixties with a high blond beehive. She’s seen every trend come and go. She adds much needed perspective. She says they look at you and see a pillow full of milk and have a way of making everything seem like an emergency. You don’t have to play along, she said. She took Lake and swaddled him up tightly and placed him in the bassinet, and got me a hot pack and an abdominal binder, and let me sleep all night.
Then it’s morning. The day nurse freaked out… you haven’t fed him since when? Midnight?! Well, the night nurse was fine with it. We had the feeling she’d seen a lot of babies survive over the years. We got him on the breast for his colostrum breakfast around 9:30am. Lake took it all in stride. He passed his final bilirubin check by the RN with the essential tremor who offered him a pacifier with sugar on it to sooth him for his heel stick. I was really surprised this was offered, and adamant that he not receive this. Instead I vigorously shushed him and kissed his face throughout, then breastfed him directly afterwards. He did great.
Discharge day! I’m not accustomed to being on the patient side of the discharge process. Of course I could relate, but its hard to be a patient patient after the OB and the pediatrician come in super early and say you’re cleared to go home. But all the paperwork and the RN teachings, and the communication among the team, of course turns it into an all day affair. We have our celebration lunch in our room, which at this point I’ve been in non-stop for days on end. I start getting ICU induced dementia. I just about leave AMA when the carseat straps can’t be adjusted to fit his shoulders and chest snugly enough on their smallest setting. I’m a raving crying wreck. Finally, we are cleared to go home around dinnertime.
Home at last.